17 November 2023
Kidney stone surgeries, including lithotripsy, are associated with a risk of postsurgical infections. According to the National Institutes of Health, an estimated 600,000 kidney stone operations were performed in the US last year. Of those, about 42,000 patients contracted an infection. Some of these infections, known as “septic events,” can be life threatening. These severe infections occur when microorganisms spread from the bladder to the bloodstream. A septic event is a medical emergency that requires hospitalization. “One big misunderstanding is just how common it is,” says Nick Sanford, vice president of medical affairs at MicroGenDX.
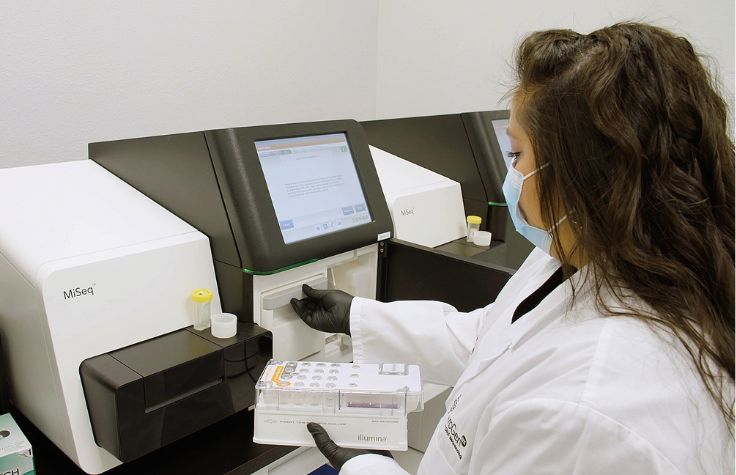
Based in Lubbock, Texas, MicroGenDX is a 200-employee lab focused on diagnostics for challenging infections. It receives samples from all over the US and the globe and runs about 2000 samples per week. Through his work, Sanford hears countless stories of people who went for an outpatient day surgery but ended up in the ICU. After his own mother had a lithotripsy in 2019, she had to be sent to the hospital to get treated for an E. coli infection. Following treatment, her culture tests came back negative, but she remained in the hospital with the same septic symptoms. “Because the cultures were clear, they said it was no longer an infection but ICU delirium, and that made absolutely no sense to me,” Sanford says. He fought for a month to get a sample from the hospital, which wasn’t yet contracted with MicroGenDX. When they finally obtained some samples, they used next-generation sequencing (NGS) and found vancomycin-resistant Enterococcus in them, which standard methods had missed. With a new treatment, she recovered in three days and went home.
Prophylaxis with an antibiotic is considered clinical best practice to nip these potentially serious infections in the bud. When a patient goes in for a kidney stone operation, the standard procedure requires taking a urine sample to determine whether they have an active infection or are at high risk for a postoperative infection. The sample is sent for culture-based testing to determine which antibiotics, if any, should be prescribed for a one-time, presurgical dose to reduce the risk of serious infection after the procedure. Unfortunately, urine culture has its limitations.
“The vast majority of those samples are going to come back culture negative or culture inconclusive,” explains Craig Tipton, director of biostatistics at MicroGenDX. “And so, what your doctors or your treating team are left to do is look at the empiric recommendations and guidelines for someone who fits a demographic mold. ‘What antibiotics should I give someone in this category?’” For stone surgeries, it’s often cefazolin, but Tipton says that drug is ineffective for some people.
Urological oncologist Dr. Michael Liss has witnessed this in his own practice at The University of Texas Health Science Center at San Antonio. “The greatest challenges our patients face today in terms of diagnosis and management are intricately tied to the risks of infection and the alarming rise in antimicrobial resistance patterns,” he says.
Challenging the current standard of care
From December 2019 to January 2022, MicroGenDX worked with Liss to determine whether NGS microbial profiling could aid in the selection of prophylactic antibiotics and actually reduce infections. Liss was the lead author on the study, which was recently published in European Urology Open Science.
The comparative efficacy trial involved two arms of 157 urologic stone lithotripsy patients, all with negative culture test results. One arm followed the standard-of-care procedure and was prescribed antibiotics without any genomic data or information to guide the choice. The second arm of patients had NGS testing to guide their selection of a prophylactic antibiotic regimen. An infectious disease pharmacist looked over the NGS results to help with the recommendations.
In the standard-of-care patients, the infection rate was 8.5%. Among the NGS-guided intervention arm, there were zero infections for those for whom the protocol was followed. (There was one instance of a doctor who did not prescribe the NGS-guided antibiotic in the intervention arm, and the patient got an infection. An intent-to-treat analysis including this patient still found the 1.3% infection rate significantly lower.)
While NGS testing adds cost to the standard urine culture, its value may be demonstrated in other ways. The paper revealed that the MicroGenDX assay costs $249, but a septic event increases the cost of ureteroscopy by $31,843. Sanford calculates that a medium-sized hospital performing about 1000 lithotripsies per year could save, after the cost of NGS testing, about $1.5 million. NGS testing could also reduce risk, time, and patient suffering.
Tipton says that prescribing antibiotics using only empirical guidelines can be boiled down to “a really good high-probability guess. I think you can move past the guesswork using NGS.”
Culture-independent testing may also help urologists and microbiologists learn more about the biology of infections. While men are more likely to need a kidney stone operation, the study authors found that women were ten times more likely to develop a postoperative infection. “That was a bit shocking to me,” says Tipton, who was one of the authors. There’s a dramatic difference in the number and types of microbes in women’s microbial profiles compared to men. “It makes a lot of sense that the same empiric antibiotics that work for men don’t work nearly as well for women.”
The study found that NGS-guided treatment supported more personalized and diverse use of antibiotics. There was a 9.3% increase in antibiotic use and an 8.1% increase in instances where two antibiotics were used at once, compared to the group that did not receive NGS testing—which may seem counterintuitive for antibiotic stewardship. However, Liss explains that this group’s 8.5% reduced risk of infection reveals a tradeoff: “By identifying pathogens more rapidly and accurately, NGS helps us prevent unnecessary or ineffective antibiotic treatments, reducing the risk of resistance development. It is an essential tool in our arsenal for early detection and targeted management.”
The growing AMR crisis
Antimicrobial resistance (AMR) refers to microbes’ ability to resist, often through mutation, antibiotics or other drugs—rendering them ineffective. This makes infections harder or impossible to treat with the limited set of currently approved pharmaceuticals. Historical overuse of some of these medications is thought to have created an environment that makes the emergence of antimicrobial resistance more likely. Antibiotics, intended to be a solution to infection, are becoming part of the problem: Organisms harboring this resistance are more likely to spread in environments like hospitals.
Sanford reflects on the broader implications of his own mother’s experience with a postsurgical infection: “Not only did they change her antibiotics, it also changed the way they handled her as a patient, because patients with VRE are put on contact precautions so it’s not spread around to other patients. Having that test probably not only saved her, but could have saved a few other patients in neighboring rooms.” For him, the entire experience underscored the importance of NGS. “I never thought when I dropped her off at the doctor that day that it would become an ICU stay. So I saw the power of the technology back then, and I’ve been a big proponent ever since.”
The World Health Organization recognizes World AMR Week November 18–24, with the theme “Preventing antimicrobial resistance together.” It estimates that almost 5 million deaths were associated with bacterial AMR in 2019, including 1.27 million deaths directly caused by it.
It will take an interprofessional village
Liss believes that the key to preventing infection and AMR is using both NGS and a cross-functional team. “The integration of NGS-guided modifications to antimicrobial prophylaxis [in our study] demanded a coordinated effort involving microbiologists, clinicians, and pharmacists,” he says. “By fostering this collaboration, we were able to strike a balance between the rapid advancements in diagnostic capabilities and the responsible use of antibiotics.”
Liss is currently applying for a grant to expand the study to multiple centers, with added goals such as collecting actual kidney stone samples for concordance testing and, ideally, implementing a framework to track patient costs, hospital resource use, and more.
“This experience has reshaped our vision of the future, particularly in terms of how we envision diagnostic stewardship in our practice,” he says.
With the help of studies like Liss’s, the research and medical communities are increasingly adopting NGS. In early 2024, MicroGenDX will be expanding from a 7000-square-foot lab to a facility with more than 20,000 square feet. Better diagnostics are on the way, and NGS-based testing may have a role to play.


