Accurate Identification of Clinically Relevant Cancer Biomarkers Paves the Way for Personalized Medicine
Introduction
The first time Ravindra Kolhe, MD, PhD. learned about next-generation sequencing (NGS) was in graduate school. “We heard about this technology that would enable us to sequence everything,” Dr. Kolhe stated. “We thought that soon we wouldn’t need to perform Southern Blots anymore.” He hoped to have the opportunity to see NGS in action during his pathology residency in 2008. Yet, it was another four years before he would have the chance to work with the technology.
In addition, to his roles as Associate Professor and Associate Director of the residency program in the Department of Pathology at the Medical College of Georgia (MCG) at Augusta Univeristy, Dr. Kolhe is also the Medical Director of the Augusta University Medical Center’s Cytogenetics Laboratory and Director of the Georgia Esoteric and Molecular Laboratory. In 2012, his team began to assess the use of NGS to identify clinically relevant disease biomarkers. “We started with biomarkers associated with inherited diseases and slowly moved toward oncology,” Dr. Kolhe said. “In cancer, the first utility was in acute myeloid leukemias. Slowly, new biomarkers have been identified in solid tumors.”
Today, Dr. Kolhe and his team are at the forefront of performing clinical trials with new biomarker panels, such as TruSight Tumor 170. iCommunity spoke with Dr. Kolhe about the advantages of large biomarker panels, the democratization of NGS, and how he sees the technology empowering research and clinical care in the future.

Q: How did you become interested in pathology?
Ravindra Kolhe (RK): Pathology was a field where I could continue my passion for research and move from more basic science to translational or clinical research. It’s also a great platform where you can interact with other medical subspecialties, such as cardiology, oncology, and pediatrics.
Q: You have many roles at MCG and the Augusta University Medical Center. Which one do you enjoy the most?
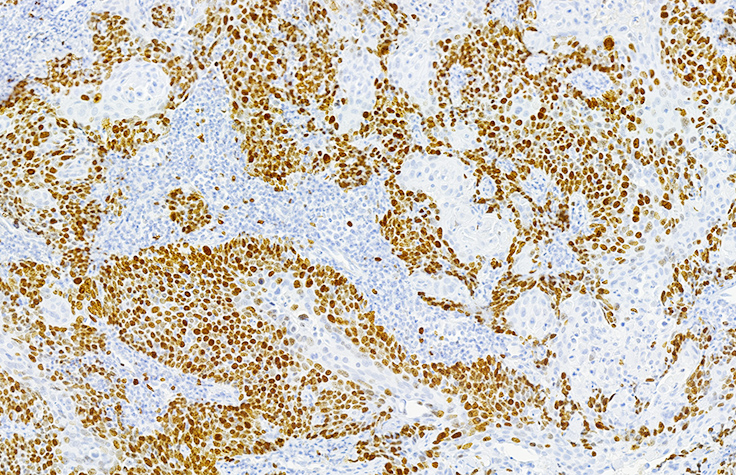
RK: I enjoy molecular pathology the most because it enables me to work with new technologies and biomarkers. There’s a significant gap between the platforms that are used in research and the ones used in translational research and clinical labs. A simple PubMed search done today would yield hundreds of biomarkers thought to be associated with breast cancer or any cancer. Yet studies of those markers yielded varied results depending on which testing methods or technologies were used. In the past 10-15 years, the only clinically validated markers in breast cancer have been ER/PR1 and HER22. NGS and other cutting-edge technologies now offer translational researchers with a reliable platform to identify which new markers have utility in clinical diagnostics. There are many more to be studied.
"It's the first large, comprehensive panel enabling us to look at a wide number of variants associated with solid tumors in a single assay."
Q: Before you began using NGS in your lab, what technologies or methods were you using to study potential biomarkers?
RK: We were performing single-gene assays for c-KIT3 mutations, FLT34, CEBPA5, and NPM16. We used karyotyping techniques such as FISH7, and molecular techniques such as PCR-based Sanger sequencing and PCR-RFLP8 genotyping. Once we brought NGS into the lab, we began performing studies with 15-, 24-, and 54-gene panels.
Q: What prompted you to begin using the TruSight Tumor 170 panel
RK: TruSight Tumor 170 is a complete platform. It offers a simple protocol for analyzing fresh, frozen, and formalin-fixed, paraffin-embedded (FFPE) tissue samples. It has integrated reagents and built-in bioinformatics.
What’s most impressive is the content and comprehensiveness of the TruSight Tumor 170. It encompasses oncology genes associated with many different solid tumors. The small panels we had been using were DNA or SNV-based and focused on markers associated with one or two solid tumor types. TruSight Tumor 170 enables us to analyze 170 genes associated with more than 14 different solid tumors. It analyzes DNA and RNA for fusions, splice variants, insertions/deletions, and SNVs.
It’s also cost effective compared to single-gene or smaller panels. It’s the first large, comprehensive panel enabling us to look at a wide number of variants associated with solid tumors in a single assay. It’s the difference between looking through a window on a starry night versus viewing the sky with the Hubble Space Telescope. TruSight Tumor 170 provides granular information on a large scale.
"We've found the TruSight Tumor 170 App to be a solid bioinformatics pipeline."
Q: What’s the advantage of looking at so many variants simultaneously?
RK: The advantage of comprehensiveness is economic, more than scientific. In clinical trials, the energy, time, and technologist cost are about the same whether we run a large or small panel. However, with smaller panels we have to guess what type of tumor might be present in the sample. We don’t have to know the solid tumor type with the TruSight Tumor 170 because it covers so many solid tumor markers. It enables us to seek answers to multiple questions in one assay.
Q: What’s been your experience analyzing the data in BaseSpace Sequence Hub with the TruSight Tumor 170 App?
RK: Data analysis with the TruSight Tumor 170 App is excellent. A few months ago, we formed the Sequoia Group with other laboratories performing sequencing and informatics in the academic space. Many within the group are now using TruSight Tumor 170. Because we’re not all bioinformaticians, the group gives us the opportunity to discuss our use of the TruSight Tumor 170 App, as well as the panel. We’ve found the TruSight Tumor 170 App to be a solid bioinformatics pipeline.
"Solutions like TruSight Tumor 170 will enable us to perform clinical trials to identify the presence of different drivers and uncover markers that could inform personalized, precision oncology."
Q: What are the potential advantages of the TruSight Tumor 170 panel in translational research?
RK: In the past, we’ve made assumptions and used a ‘one size fits all’ method of treating cancers. We had specific therapy regimens for certain cancers and that’s what we’d use. We never considered or investigated what was driving oncogenesis, how those drivers could vary in different people, at different stages of disease, or in relapse. We’re one of many groups who are now focused on identifying those differences to support the move toward an individual tumor genetics driven methodology for treating cancer. Solutions like TruSight Tumor 170 will enable us to perform clinical trials to identify the presence of different drivers and uncover markers that could inform personalized, precision oncology.
Q: From a training standpoint, how long did it take your team to become proficient performing the assay with the NextSeq 550 System?
RK: We did our homework before the training, dissecting the protocol and creating our own run sheet. By the time the Field Application Specialist came to train us, we were ready with questions. It made a huge difference. We watched the FAS perform the first run. My team performed the second run independently, and then we were on our own. The NextSeq 550 System is easy to use. We’ve seen 100% data concordance between technicians.
Q: What have been the benefits of working with the Illumina team?
RK: The Illumina team has been amazing. They understand the studies we’re performing and have been very helpful.
It’s the people who really make the difference and why we want to work with one company versus another company. Science is great, but you want to work with a team that’s supportive. We’re spending time, energy, and money with a company and its products. We need them to be good listeners.
Q: What does the term “the democratization of NGS” mean to you and your lab?
RK: It means that NGS isn’t restricted to a reference lab, large labs, or academic centers. In the future, I think NGS will become a routine platform in every research or clinical laboratory. As protocols become more sophisticated, automated, and easy to use, NGS assays will become just another test. As the cost of sequencing goes down, and payors understand the value, reimbursement levels for NGS panels will be established, and more laboratories will begin offering them.
Q: What will NGS empower in the future?
RK: We haven’t begun to approach what NGS is capable of delivering. We started with 15-, 26-, and then 54-gene panels. Now we have TruSight Tumor 170 and consider it a large panel. Yet, there will be even larger panels in the future. At some point we’ll shift to clinical whole-exome, low-pass clinical whole-genome, and then clinical whole-genome sequencing. We’re not there yet, but we’re heading there.
Footnotes
- ER/PR, estrogen receptor/progesterone receptor
- HER2, human epidermal growth factor receptor-2
- c-kit, tyrosine-protein kinase kit
- FLT3, Fms-related tyrosine kinase 3
- CEBPA, CCAAT enhancer-binding protein alpha
- NPM1, nucleophosmin 1
- FISH, fluorescent in situ hybridization
- PCR-RFLP, PCR-restriction fragment length polymorphism